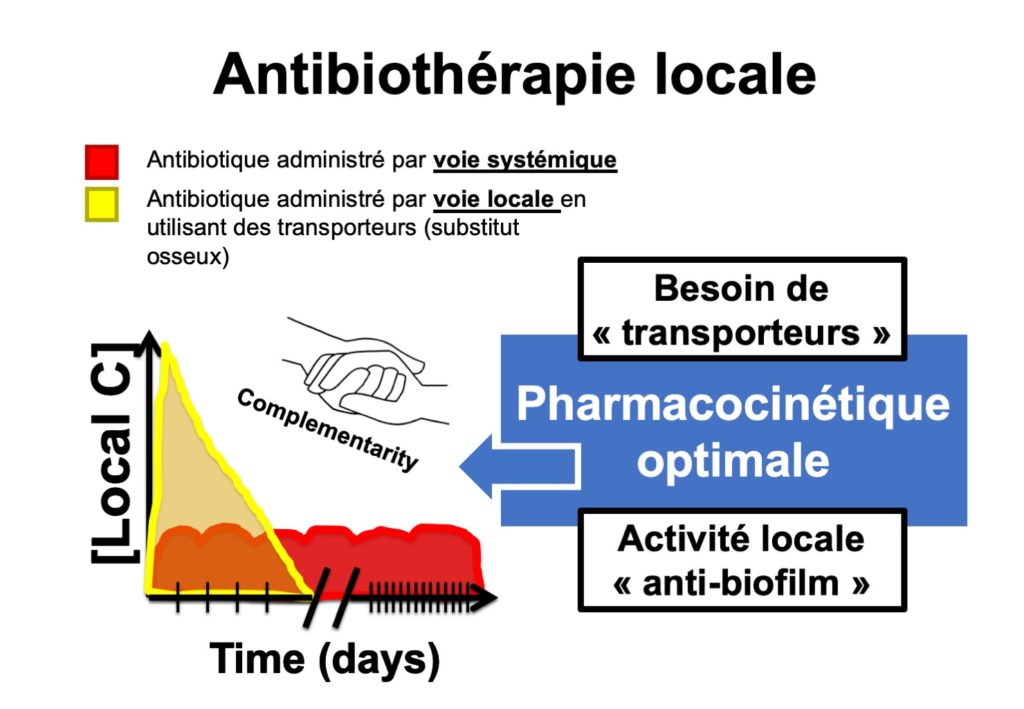
Principle of local antibiotic therapy
Principle of bone substitutes
A bone substitute is a device generally made of calcium sulfate and hydroxyapatite. It is presented as a paste, in a syringe. Its primary purpose, is to promote bone remodeling, i.e. the “regrowth” of bone. By filling the gap, this network of calcium sulfate and hydroxyapatite can thus provide a setting for colonisation by the bone cells of the individual. Bone substitutes available on the market have obtained European Commission (CE) marking. Some manufacturers have added antibiotics, such as gentamicin or vancomycin, to the composition of the bone substitute. These antibiotics are stable in the bone substitute. They are delivered in high concentrations over several weeks.
The standard treatment for chronic osteomyelitis is to get rid of bone sequestration and bacteria, in the form of biofilm, present in the intramedullary area, to identify the bacteria involved, and to treat with systemic antibiotics for a period of 3 months. The use of a bone substitute in this indication helps to :
- fill the cavity, and thereby avoid superinfections,
- deliver locally high concentrations of gentamicin, which has a broad spectrum of activity on staphylococci, streptococci and enterobacteria, and is synergistic with systemically-administered antibiotics,
- promote bone remodeling, i.e. colonisation of the gap by bone cells to facilitate repair.
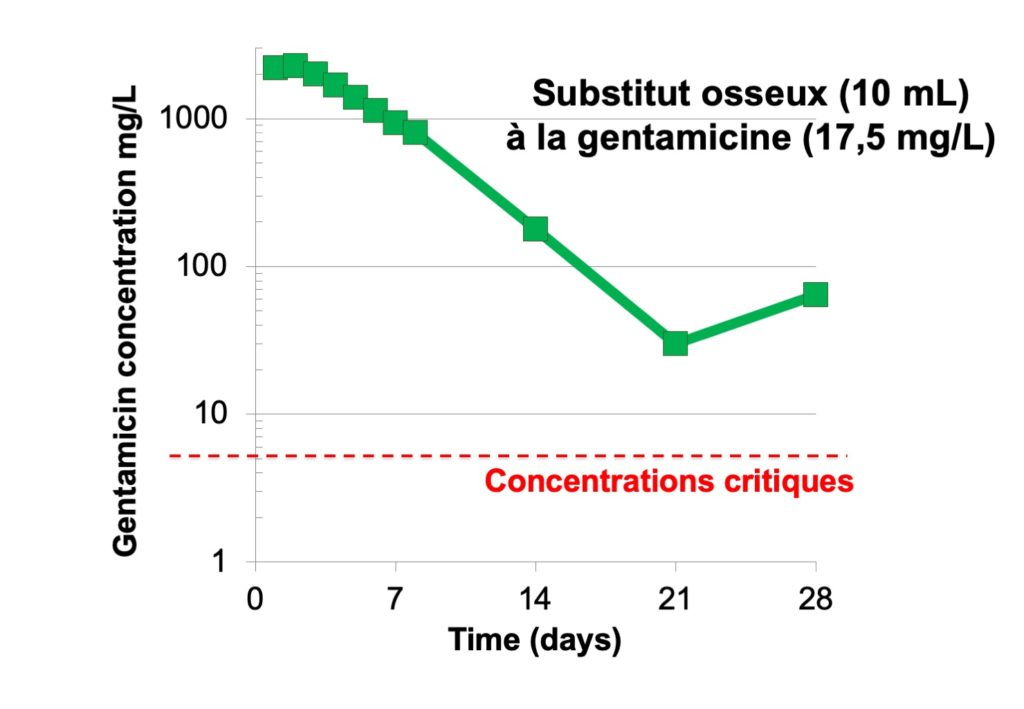
Example of pharmacokinetics resulting from gentamicin released by bone substitute, with very high local concentrations (logarithmic scale), far above bactericidal concentrations, for more than three weeks
Acute osteomyelitis of the humerus at the age of 12 was left untreated. Twenty years later, Brodie’s abscess is visible (area of osteolysis in humeral diaphysis) on x-ray and MRI. When there is an indication of corticotomy, a gentamicin bone substitute can be used. Thus the cavity can be filled, high concentrations of antibiotic can be delivered locally, bacterial superinfection can be avoided, and bone remodeling can be promoted.


